New target for new outcomes
IBD is no longer seen as a simple inflammatory disease but a rather complicated disorder of intestinal components including epithelial cells, immune cells, neural cells, and extracellular matrix. Particular types of microbes, environmental factors including sanitary conditions and food, and genetic factors are also suggested to be involved. Major advances in understanding the pathophysiology of fibrosis in the gut and in the identification of new antifibrotic targets have occurred in the past few years.
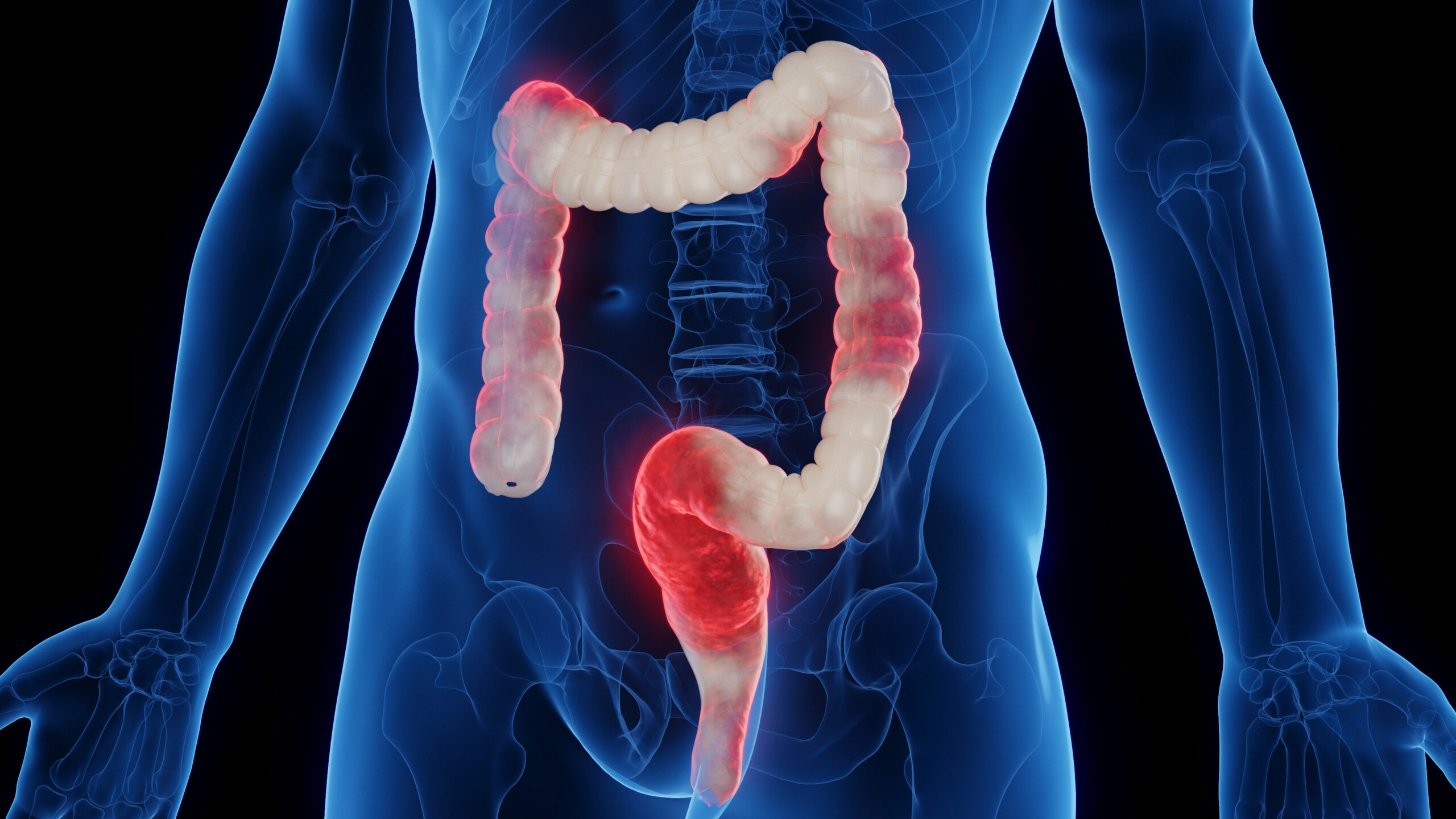
Intestinal fibrosis, which is characterized by excessive deposition of ECM components by activated cells of mesenchymal origin in the intestinal wall, is the basis of several gastrointestinal disorders, in particular IBD, namely Crohn’s disease (CD) and ulcerative colitis (UC). Consequently, intestinal fibrosis has become a target to achieve adequate endoscopic improvement.
GUT-1 : a new approach to treating IBD
GUT-1 is an RNA oligonucleotide that silences the carbohydrate sulfotransferase 15 gene.
Activated fibroblasts located in submucosa express CHST15, which produces a highly sulphated matrix – chondroitin sulfate E (CS-E). CS-E creates stroma rich microenvironment in UC/CD and causes excessive fibrosis. Submucosal fibrosis directly links with severity of mucosal inflammation, which cannot be treated with previous biologics such as IFX and VDZ (REF 1-2). Submucosal fibrosis can lead to UC-related symptoms such as loose stools, diarrhea, abdominal discomfort, pain and tenesmus, and to IBD-related complication, stricture which may require surgery (REF 3). GUT-1 suppresses the production of CHST15 and CS-E, which in turn represses submucosal fibrosis and contributes to inhibit fibrosis-associated persistent inflammation and symptoms.
What is IBD?
IBDs such as Crohn’s disease and ulcerative colitis are characterized by uncontrolled activation of intestinal immune cells in a genetically susceptible host. Due to the progressive and destructive nature of the inflammatory process in IBD, complications such as fibrosis, stenosis or cancer are frequently observed, which highlights the need for effective anti-inflammatory therapy. Studies have identified altered trafficking of immune cells and pathogenic immune cell circuits as crucial drivers of mucosal inflammation and tissue destruction in IBD. A defective gut barrier and microbial dysbiosis induce such accumulation and local activation of immune cells, which results in a pro-inflammatory cytokine loop that overrides anti-inflammatory signals and causes chronic intestinal inflammation (REF 4).
References:
- Arijs I, De Hertogh G, Lemmens B, et al. Effect of vedolizumab (anti-α4β7-integrin) therapy on histological healing and mucosal gene expression in patients with UC. Gut. 2018 Jan;67(1):43-52.
- Gundersen MD, Goll R, Fenton CG, et al. Fibrosis Mediators in the Colonic Mucosa of Acute and Healed Ulcerative Colitis. Clin Transl Gastroenterol. 2019 Oct;10(10): e00082.
- Gordon IO, Agrawal N, Willis E, et al. Fibrosis in ulcerative colitis is directly linked to severity and chronicity of mucosal inflammation. Aliment Pharmacol Ther. 2018 Apr;47(7):922-939.
- Markus F Neurath. Targeting immune cell circuits and trafficking in inflammatory bowel disease. Nat Immunol. 2019 Aug;20(8):970-979.